What does it take to be an outstanding trust board in an ICS?
13 December 2021
GGI executive partner Darren Grayson suggests that the CQC well-led framework key lines of enquiry might be useful for NHS trusts that want to be outstanding ICS partners.
Up and down the country ICS leaders are busy refining system development plans and constitutions, ensuring they are “ready to operate” as statutory ICSs in April 2022.
But what is the role of NHS trust boards at this time, beyond engaging in the system conversations and plans? For ICSs to thrive, NHS trust boards need to formally evaluate their own readiness to operate in a system and commit to stepping up their game.
We suggest that trust boards use the well-led framework for this purpose. Although the CQC does not seem to have progressed its plans to regulate on a system basis, forward thinking trusts that want the best for their local communities will be considering this step.
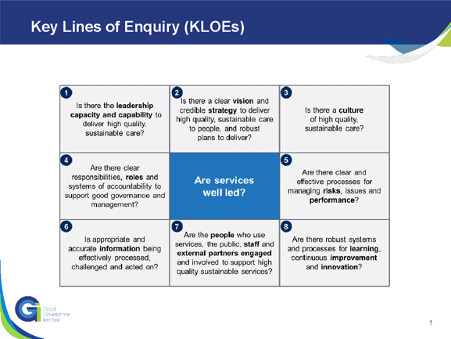
The CQC well-led framework sets out eight key lines of enquiry (KLOEs). Below we highlight the characteristics of trust boards that are, or plan to be, outstanding ICS partners.
Leadership capacity and capability
The trust’s leadership strategy is based on principles of collective and distributive leadership, there are joint leadership development programmes with other system partners, and a culture of joint posts and development opportunities across partners. Senior leaders commit to system roles and responsibilities, seeing these as part of the day job rather than an added extra.
Vision and credible strategy
The trust’s vision is outward rather than inward-looking - not aiming to be ‘the best hospital in the country’ but making a difference to the lives of the communities they serve. The strategy adopts or is aligned with the triple aim of improving patient experience, improving population health, and improving value. More importantly, there are credible, SMART plans in place to achieve improvements in population health rather than vague statements of intent.
Culture
Leaders role-model the importance of developing networks and relationships across the system, and make decisions in the interests of the population. Words such as partnerships, communities, integration and collaboration are heard in the discourse across the organisation. Examples of when the trust has made a decision in the interests of the local community, rather than the organisation, are clear and communicated widely.
Responsibilities, roles and systems of accountability
Responsibilities for integration and partnerships are weaved through the portfolios of the senior leadership team and boards have actively considered development of capacity through specific roles and teams. On a similar note, the governance arrangements, including board committees, should have reviewed their terms of reference and annual cycle of business in order to incorporate issues related to system-working. A time-limited working group could have been set-up to guide this development and ensure focus. And new leadership skills will have been developed, based on collaboration and seeing the big picture, rather than competition. Systems of accountability will be in place - for the system rather than for one organisation or trust.
Managing risks, issues and performance
Linked to the development of an outward-focused vision and strategy, the board assurance framework has been made more outward-facing and aligned with the major system risks, with evidence that the trust is playing its part to mitigate risks associated with the wider determinants of health. On the flip side to this, management of issues and performance should routinely consider the external causes and how system partners can be engaged in finding and implementing solutions.
Appropriate and accurate information
Many trust boards may receive an update about systems issues in the CEO’s report, as well as periodic papers. A good board should receive standing reports on system development and performance. Quality, finance and workforce reports should include metrics related to the wider determinants of health, health inequalities and the role as an anchor institution, with clear actions and recommendations.
Engagement and involvement
The Trust has effective methods to engage all members of its local communities and seeks their feedback on services and provides them with the opportunity to become involved. The trust should have agreed a strategy for developing partnerships and be able to evidence how it is supporting system partners such as primary care and the VCSE through structured programmes of engagement and practical support.
Learning, continuous improvement and innovation
The trust promotes involvement in system research and innovation programmes, as well as networks, and supports staff to take on these roles and responsibilities. Quality improvement methodologies should be used to tackle system issues, with dedicated improvement programmes set up with local partners to improve population health and address health inequalities, and participation in system-wide improvement collaboratives.
Step change
No one is expecting trusts to have all of the above in place immediately. The move to integrated care represents a journey towards a very different place to the familiar culture and working practices of trust and leadership that have been in place since the internal market was created in the early 1990s. It will not necessarily be an easy journey and trusts may need support to conceive and develop the new culture and ways of working that will be needed. GGI is ready to offer that support.
